Did you know that there are more than 70 different terms for functional voice disorders? Some of these include psychogenic, conversion and even the much older terminology of hysterical dysphonia from the 1800s – let’s move on from that! Some of the more contemporary
There are many types of functional neurological disorders including those that affect movement, swallowing, voice and even blindness. The focus of this article is on functional neurological voice disorders, also known as functional voice disorders.
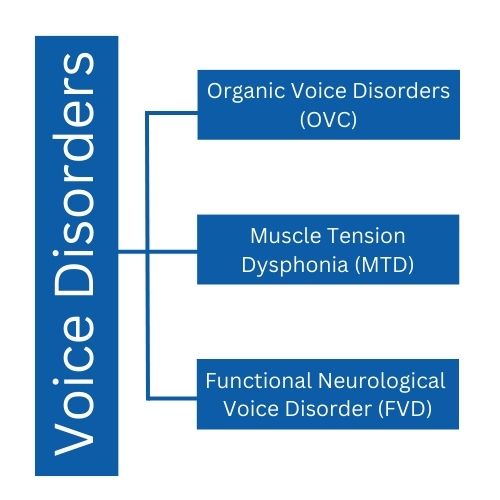
Organic vs Muscle Tension vs Functional Voice Disorders
The Payten et al (2022) “Recommended Framework for the Classification of Voice Disorders” suggests three categories; organic voice disorder, muscle tension voice disorder and functional voice disorders. It is helpful to have an understanding of the differences between them.
An Organic Voice Disorder means that you can see something physically wrong with the voice box (larynx) from injury or disease like a cyst, a haemorrhage, paralysis, or abnormal structures such as a laryngeal web.
Muscle Tension Voice Disorder is all in the name. The muscles associated with voice production experience tension and tightness which affects their ability to produce voice efficiently. The voice sounds and feels excessively strained, tense and is sometimes painful. Producing voice is effortful, and the person feels like they are ‘pushing from the throat’. The result of this is that the voice fatigues quickly.
The build-up of muscle tension can be from a variety of issues including:
- posture (do you talk with the phone between your ear/shoulder?)
- work, emotional, physical, domestic loads (carrying the weight of the world?)
- environment (do you continually speak over background noise or across large distances without correct amplification)
- life events and difficulties (eg. grief, change, abuse)

The tightness can be seen on a nasendoscopy/stroboscopy as the false vocal folds are contracting instead of being relaxed and creating an open airway. This can limit vibration of the true vocal folds, reduce resonance and restrict airflow.
Muscle Tension Dysphonia is an inefficient way of making sound, that in time can lead to physical changes causing a secondary Organic Voice Disorder like nodules.
- Effective treatment will combine strategies to de-constrict the muscles as well as considering the causal factors.
- Laryngeal massage by a trained Speech Pathologist +/or Physiotherapist can also be helpful.
A functional neurological voice disorder or just functional voice disorder (FVD) is when the activity (function) of speech control is impacted, even though there is no obvious cause of this poor function of the voice. In ‘computer’ terms, the hardware works, but the software has a glitch.
FVD sits under a larger umbrella term of Functional Neurological Disorder with varied symptoms including; limb weakness, stuttering, word finding, swallowing, and dissociative (seizure-like) episodes. Short, easy to understand videos for patients can be found at Functional Neurological Disorder (FND) – A Patient’s Guide to FND.
Functional Voice Disorders in the Community
It is interesting to consider just how prevalent voice disorders are in the general population and who is most likely to be affected. In an Australian study by Baker et al 2013, the following summary provides a snapshot of those who are impacted by different forms of voice disorders.
- Women consist of 71% of voice referrals to Bayside Voice Centre consistent with 76% global data indicated by Morton and Watson, 1998 (possibly due to more women presenting for medical care).
- It is more common for women with FVD to be older (average age 50yrs), have lost both parents, have lower levels of tertiary education, and less are in management roles compared with women with MTD.
- A person experiencing FVD can present with various levels of severity from no voice at all (aphonia), to consistent or intermittent changes to the voice quality (dysphonia).
- However, more Men present with an OVD (e.g. a vocal fold haemorrhage, lesion) and are 7 times more likely to have laryngeal cancer with demographic risk factors of age, smoker, alcohol consumption, lower education and socio-economic status.
Initially, we might wonder if a functional voice disorder diagnosis means, ‘they just don’t know what the cause is’, and it does take in-depth interviewing and investigation to consider all pieces of the voice puzzle. When you come for an initial appointment at Bayside Voice Centre, we ask about these topics on our ‘Client Case History Form’. The information collected and your initial assessment guides an accurate diagnosis and treatment approach based on researched data. While misdiagnosis of functional voice disorder can be common, the correct diagnosis is important because the treatment approaches vary depending on the type of disorder.
Possible contributing factors that link to the prevalence of various voice disorders include:
- gender
- breathing
- reflux
- environmental conditions
- physical stressors
- emotional load
- education level
- culture
- job
- access to health care
- social support
- autonomy
- genetics
- family load
- life events
For some people, the impact of one large event, cumulative events, +/or a variety of biological, social, and psychological factors can trigger the brain into a fight/flight/freeze response that changes the voluntary control over their voice. There does NOT need to be a significant, psychologically, distressing event before the onset of the functional voice disorder, however recent data shows some people share common factors.
- Some report feeling the PITS – Powerlessness In The System (eg. this could be at work or could be trying to navigate/access health, education or other government systems).
- Others feel ‘COSO’ – Conflict Over Speaking Out if they do, or if they don’t speak out.
- Some describe the ongoing impact of life events and difficulties (eg. grief, change, abuse, illness, injury) and giving more focus to thoughts of what might happen.
- Some are progressively overwhelmed by everything on ‘the list’ – the cascading, emotional, physical, domestic loads women often carry.
- Then others will arrive without any voice, yet report none of these patterns.
What we notice during the assessment and intervention process for FVD is that automatic, pre-verbal, non-speech is still intact and can help the person to recover their voice, e.g. laugh, cough. On the other hand, the person has very limited voluntary control over their intentional speech.
FVD is extremely frustrating for the speaker since there is a big discrepancy between what their vocal folds appear to be able to do (physical appearance on scope) and how severe they actually sound. Family, friends and colleagues can also be confused if they hear the person with FVD sound better one moment then very disordered the next. The person themselves may start to wonder ‘am I making it up?’.
The short answer is NO. This is a very real issue.
You can tell when your bestie feels excited, irritated or tired just from the tone of their voice because it is natural for our body to reflect emotions. Supporting someone with a FVD involves reassurance that the problem exists and seeing a Speech Pathologist with experience in voice.
The Speech Pathologist uses a combination of voice therapy and counselling techniques in collaboration with a medical team for holistic diagnosis and management. Counselling with your Speech Pathologist can help explore if any events or stressors link with vocal +/or with a Psychologist for expertise to further unpack these issues.
Other Types of Functional Neurological Voice Disorders
In addition to the functional voice disorders mentioned above, there is also Puberphonia which is experienced by men who maintain a higher pitch after puberty.
Help with Functional Voice Disorders
The good news is that you don’t have to struggle with functional voice disorders on your own. There is help available. The correct diagnosis is important when determining the treatment options that will be most effective. For this reason, seeing the right professionals is extremely important.
At Bayside Voice Centre we provide a holistic view to your health care and recognise the need for collaboration with a team of medical professionals. As a Certified Practising Speech Pathologist, Jenny has a special interest and experience in the area of voice. To make an appointment to consider possible functional voice disorder treatment approaches, please call (07) 3193 5436.
For more information
References
Dr Janet Baker, David I. Ben-Tovim, Andrew Butcher, Adrian Esterman & Kristin McLaughlin (2007) Development of a modified diagnostic classification system for voice disorders with inter-rater reliability study, Logopedics Phoniatrics Vocology, 32:3, 99-112, DOI: 10.1080/14015430701431192 Read Article
Janet Baker (2010) Women’s voices: Lost or mislaid, stolen or strayed?, International Journal of Speech-Language Pathology, 12:2, 94-106, DOI: 10.3109/17549500903480060 Read Article
Janet Baker, David Ben-Tovim, Andrew Butcher, Adrian Esterman & Kristin McLaughlin (2013) Psychosocial risk factors which may differentiate between women with Functional Voice Disorder, Organic Voice Disorder and a Control group, International Journal of Speech-Language Pathology, 15:6, 547-563, DOI: 10.3109/17549507.2012.721397 Read Article
Baker, J. (2017) Psychosocial Perspectives on the Management of Voice Disorders. Implications for Clients: Options and Strategies for Clinicians. Compton Publishing Ltd. GB
Christopher L. Payten, Greg Chiapello, Kelly A. Weir, Catherine J. Madill. (2022) Frameworks, Terminology and Definitions Used for the Classification of Voice Disorders: A Scoping Review, Journal of Voice, ISSN 0892-1997, https://doi.org/10.1016/j.jvoice.2022.02.009. Read Article



